Introduction of Major Health Programmes in India
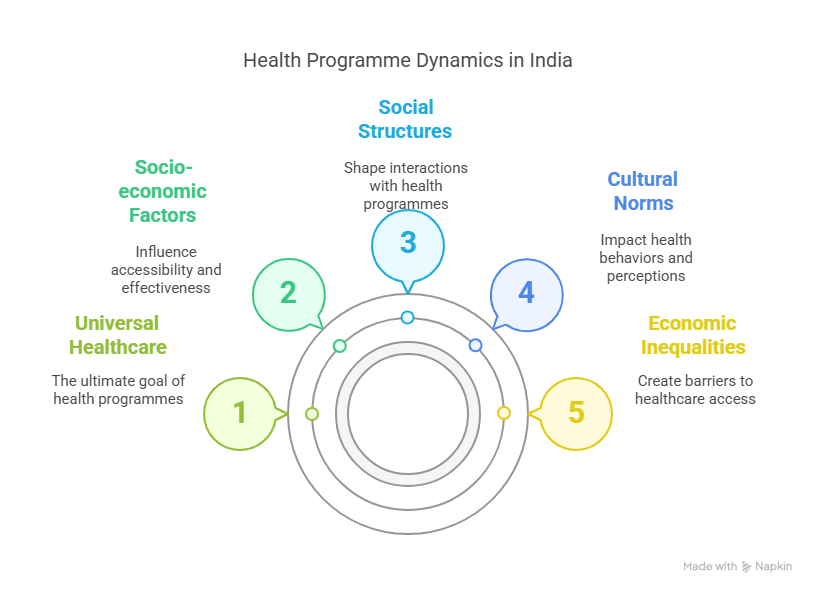
In India, health programmes are designed not only to address medical concerns but also to tackle socio-economic disparities that affect healthcare accessibility. The sociological perspective examines how health programmes interact with social structures, cultural norms, and economic inequalities.
India’s health policies have evolved from colonial-era initiatives to comprehensive welfare schemes aimed at universal healthcare. However, challenges such as caste, gender, rural-urban divides, and poverty continue to influence the effectiveness of these programmes.
1. National Health Mission (NHM)
Overview
The National Health Mission (NHM), launched in 2013, integrates the National Rural Health Mission (NRHM, 2005) and the National Urban Health Mission (NUHM). Its goal is to provide universal access to equitable, affordable, and quality healthcare.
Sociological Analysis
- Rural-Urban Divide: NRHM focuses on rural areas where healthcare infrastructure is weak, while NUHM addresses urban slums. However, urban health services remain fragmented due to migration and overcrowding.
- Caste and Gender Disparities: NHM emphasizes maternal and child health, but marginalized communities (SC/ST, OBC) often face discrimination in accessing services. The Janani Suraksha Yojana (JSY) under NHM promotes institutional deliveries, yet many women in rural areas still rely on traditional birth attendants due to social norms.
- Community Participation: NHM involves ASHA (Accredited Social Health Activists) workers, mostly women from local communities, bridging gaps between healthcare systems and rural populations. However, ASHA workers often face exploitation with low wages and high workloads.
2. Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
Overview
Launched in 2018, Ayushman Bharat is the world’s largest government-funded health insurance scheme, providing ₹5 lakh per family annually for secondary and tertiary care hospitalization.

Sociological Analysis
- Poverty and Healthcare Access: PMJAY targets the poorest 40% of India’s population, reducing out-of-pocket expenses. However, awareness and last-mile delivery remain issues, particularly among illiterate and tribal populations.
- Public vs. Private Healthcare: The scheme empanels private hospitals, raising concerns about commercialization of healthcare. Wealthier individuals may exploit benefits, while the poorest struggle with documentation (lack of Aadhaar, caste certificates).
- Gender Equity: While PMJAY covers women, patriarchal norms often restrict their access to healthcare, with male members prioritizing their own treatment over women’s health needs.
3. National AIDS Control Programme (NACP)
Overview
Initiated in 1992, NACP aims to prevent and control HIV/AIDS through awareness, testing, and antiretroviral therapy (ART).
Sociological Analysis
- Stigma and Discrimination: HIV-positive individuals, especially from LGBTQ+ communities and sex workers, face social ostracization, deterring them from seeking treatment.
- High-Risk Groups: Migrant laborers and truck drivers are vulnerable due to mobility and lack of awareness. Programmes target them, but societal taboos around sex education hinder prevention efforts.
4. National Tuberculosis Elimination Programme (NTEP)
Overview
Previously known as the Revised National Tuberculosis Control Programme (RNTCP), NTEP aims to eliminate TB by 2025 through early detection and free treatment.
Sociological Analysis
- Poverty and TB: Tuberculosis tends to strike hardest among those who are economically disadvantaged, largely because of insufficient nutrition and the strain of living in cramped quarters. Despite free treatment, many discontinue medication due to lack of wages during treatment.
- Stigma: TB patients often hide their condition due to fear of social exclusion, delaying diagnosis and increasing transmission.
- Urban Slums vs. Rural Areas: Slum dwellers are at higher risk due to poor sanitation, while rural populations face challenges in accessing diagnostic facilities.
5. National Mental Health Programme (NMHP)
Overview
Launched in 1982, National Mental Health Programme (NMHP) seeks to incorporate mental health services into primary healthcare, tackling the escalating mental health crisis in India.
Sociological Analysis
- Cultural Perceptions of Mental Illness: Mental health is often stigmatized, seen as a “weakness” or “supernatural affliction.” Many families avoid seeking treatment due to shame.
- Lack of Infrastructure: Psychiatrists are scarce in rural regions, necessitating that patients undertake lengthy journeys. Urban areas have more facilities, but affordability remains an issue.
- Gender Disparities: Women’s mental health is often neglected, with depression and anxiety dismissed as “normal” due to domestic pressures.
6. Immunization Programmes (Mission Indradhanush & Intensified Mission Indradhanush)
Overview
These initiatives aim to achieve 90% immunization coverage against preventable diseases like polio, measles, and hepatitis.
Sociological Analysis
- Religious and Cultural Myths: Some communities refuse vaccines due to misinformation (e.g., polio drops causing infertility).
- Migrant Populations: Nomadic tribes and seasonal laborers miss immunization drives due to mobility.
- Gender Bias: Male children are often prioritized for vaccination over female children in patriarchal households.
7. Janani Shishu Suraksha Karyakram (JSSK)
Overview
Under NHM, JSSK provides free delivery, C-sections, and newborn care to reduce maternal and infant mortality.
Sociological Analysis
- Traditional Beliefs vs. Modern Healthcare: Many rural women prefer home deliveries due to cultural practices, despite risks.
- Economic Barriers: Though services are free, hidden costs (transport, unofficial hospital charges) deter poor women.
- Patriarchal Control: Women often need male family members’ permission to seek medical care, delaying critical interventions.
8. National Programme for Healthcare of the Elderly (NPHCE)
Overview
NPHCE addresses geriatric care through specialized facilities and home-based care.
Sociological Analysis
- Changing Family Structures: Nuclear families and migration leave elderly without caregivers, increasing dependency on state support.
- Economic Vulnerability: Poor elderly lack pensions, forcing them to work despite health issues.
- Social Isolation: Widowed and disabled elderly face neglect, worsening mental and physical health.
Challenges and the Way Forward
1. Social Determinants of Health
Health programmes must address caste, class, gender, and regional disparities to ensure equitable access.
2. Community Participation
Grassroots involvement (via ASHA workers, NGOs) can improve trust and awareness.
3. Intersectional Approach
Policies should consider overlapping identities (Dalit women, tribal migrants) for inclusive healthcare.
4. Strengthening Public Health Infrastructure
Investment in rural healthcare, digital health (telemedicine), and stricter regulation of private players is crucial.
5. Behavioral Change Communication
Awareness campaigns must combat stigma around HIV, TB, and mental health using culturally sensitive approaches.
Conclusion
India’s health programmes reflect a commitment to universal healthcare, yet their success depends on addressing deep-rooted social inequalities. A sociological approach reveals how caste, gender, poverty, and cultural norms shape health outcomes. Future policies must integrate social justice, community engagement, and inclusive development to achieve Health for All.
By bridging gaps between policy and grassroots realities, India can move towards a healthier, more equitable society.

Topic Related Questions on Major Health Programmes in India
5-Mark Questions on Major Health Programmes in India (Short Answer Type)
- What is the National Health Mission (NHM)?
- Explain the role of ASHA workers in India’s healthcare system.
- What are the key objectives of Ayushman Bharat-PMJAY?
- How does stigma affect HIV/AIDS prevention under the National AIDS Control Programme (NACP)?
- What are the major challenges in implementing immunization programmes in rural India?
- How does the Janani Shishu Suraksha Karyakram (JSSK) aim to reduce maternal mortality?
- What is the sociological significance of the National Mental Health Programme (NMHP)?
- How does poverty influence tuberculosis treatment under NTEP?
- What are the key features of the National Programme for Healthcare of the Elderly (NPHCE)?
- How do caste and gender disparities impact access to healthcare in India?
10-Mark Questions on Major Health Programmes in India (Detailed Answer Type)
- Discuss the role of the National Health Mission (NHM) in improving rural healthcare in India.
- Analyze the impact of Ayushman Bharat-PMJAY on India’s healthcare system from a sociological perspective.
- Examine the challenges faced by the National AIDS Control Programme (NACP) in addressing HIV/AIDS in high-risk groups.
- How does the National Tuberculosis Elimination Programme (NTEP) address socio-economic barriers in TB treatment?
- Critically evaluate the effectiveness of immunization programmes like Mission Indradhanush in India.
- Discuss the social and cultural barriers affecting maternal healthcare under Janani Shishu Suraksha Karyakram (JSSK).
- Explain the importance of mental health awareness under the National Mental Health Programme (NMHP).
- How does the National Programme for Healthcare of the Elderly (NPHCE) address the needs of India’s aging population?
- What are the key differences between rural and urban healthcare delivery under NHM?
- How do caste and gender inequalities influence access to healthcare in India? Provide examples from major health programmes.
15-Mark Questions on Major Health Programmes in India (Essay-Type/Long Answer)
- Critically analyze the major health programmes in India from a sociological perspective, highlighting their successes and limitations.
- Discuss how social determinants like caste, class, and gender affect the implementation of health programmes in India. Provide examples.
- Evaluate the role of community participation (e.g., ASHA workers) in improving healthcare delivery under the National Health Mission (NHM).
- “Ayushman Bharat-PMJAY is a game-changer for India’s healthcare system, but challenges remain.” Discuss this statement with sociological insights.
- How do traditional beliefs and cultural practices impact the success of immunization and maternal health programmes in India?
- Examine the challenges faced by marginalized communities (SC/ST, tribal populations) in accessing healthcare under major government schemes.
- Discuss the role of public-private partnerships in India’s healthcare system, with reference to Ayushman Bharat and other schemes.
- “Mental health in India remains neglected due to stigma and lack of awareness.” Critically analyze this statement in the context of NMHP.
- Compare and contrast the rural and urban healthcare infrastructure in India, focusing on major health programmes.
- How can India’s health policies be made more inclusive to address the needs of vulnerable groups (women, elderly, disabled, migrants)?
Special Focus: COVID-19 & Health Programmes
- How did India’s health programmes adapt during the COVID-19 pandemic? (10 marks)
- Discuss the role of the PM Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) in pandemic preparedness. (15 marks)
- What were the challenges in vaccine distribution under the Universal Immunization Programme (UIP) during COVID-19? (10 marks)
